Thrombosuction with Export Aspiration Catheter during PCI in Acute MI
Shuvanan Ray1, Bhabani Prasad Chattopadhyay2, Shilanjan Roy3, Subhas Kundu4, P K Deb5, Amal Bannerjee6
Head of the Department of cardiology, A.M.R.I. Hospitals, Salt Lake, Kolkata.
Assistant Professor, Dept. of cardiology, North Bengal Medical College.
Registrar, CCU, A.M.R.I. Salt Lake, Kolkata.
HOD, Cardiology, ESI Hospital, Kolkata
Senior Consultant Cardiologist, Institute of Cardiovascular Sciences, Kolkata.
|
|
Introduction:
Primary PCI is now the most effective treatment of occluded coronary artery 1 in AMI. However dilatation of the coronary artery leads to disruption of plaque and stent-deployment results in shifting of plaque. Disruption and shifting of plaque may result in distal embolisation of plaque debris or thrombus. Situation becomes more critical if the infarct related artery is loaded with thrombus.
Slow flow or no-reflow may occur after primary PCI. Reduction of thrombus burden by thrombosuction (with or without distal protection device) in subjects pre-treated with abciximab (Gp IIb-IIIa Inhibitors) can prevent distal embolisation, improve myocardial perfusion and hence myocardial salvage.
Thrombosuction alone unaccompanied by any other additional intervention is infrequently reported2 But thrombosuction may sometimes be all that is required without further need of coronary angioplasty and stenting. The rarity of reported cases of thrombosuction alone merits highlight. Hence the present case is being discussed in the ensuing paragraphs.
Clinical Summary:
A 22 yrs old young man with strongly positive family history of coronary artery disease had inexorable chest pain of one hour duration before he presented to our hospital with diaphoresis, loss of consciousness, feeble pulse (140/min) systolic blood pressure of 70 mm Hg & tachypnoea. Both lungs were full of crepitations and LV – S3 Gallop was present. ECG showed ST elevation in V1 to V4. Echocardiography revealed gross
was one of the first bare metal stents (BMS) approved in USA. Subsequently, many more bare metal stents came on the market, but the significant problem of restenosis remained as a major issue.
In 2003, a drug-eluting stent approved by the Food and Drug Administration (FDA) set another mile stone in reduction of restenosis3. This therapeutic effect of drug-eluting stent was very impressive with consistently positive reports from subsequent small group trials and first hand experience of the physicians, which led to remarkable adoption of drug-eluting stents, even in patients where there was no approved indications. This use of drug-eluting stents was termed as an “off-label” use.
Subsequently in the years 2005 and 2006, many small reports questioned the safety of drug-eluting stents, especially late stent thrombosis. Some of the studies which prompted media attention included a BASKET-LATE 4 a study presented in the American College of Cardiology in March of 2006, and subsequently a Camenzind’s meta analysis presented at the European Society of Cardiology in September 2006. Later, there was also a publication by the SCAAR5 (Swedish Coronary Angiography and Angioplasty registry) registry group from Sweden which got immediate attention of the worldwide interventional community in cardiology. Their landmark analysis at 6 months showed no difference in mortality among bare metal stents and drug-eluting stents but after 6 months, there was increased mortality in the drug-eluting stent group. This set off a worldwide panic and Swedish government prohibited the use of drug-eluting stents unless absolutely needed, media calling the drug-eluting stents “a million ticking time bombs”
Correspondence: Dr. Shrivana Ray, Head of the Department of cardiology, A.M.R.I. Hospitals, Salt Lake, Kolkata., West Bengal, India
Email: rk1965@gmail.com
|
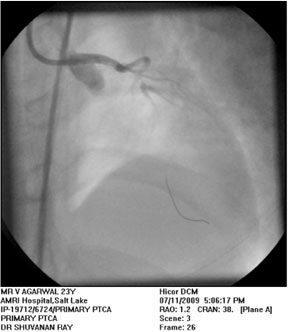 |
Figure-1. Coronary angiography before thrombosuction. LAD is thrombus laden. |
 |
| Figure-2 Placement of EAC in LAD. |
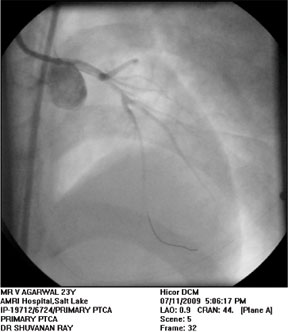 |
| Figure-3 Appearance of LAD after thrombosuction |
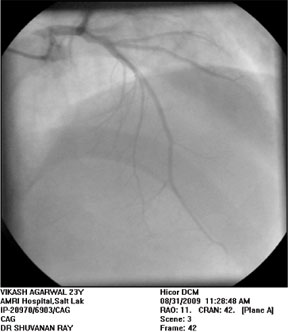 |
| Figure-4. Follow-up coronary angiography after one and a half month |
|
After angiographic visualization LMCA was engaged with a 7F extra backup(XB) guide catheter Over the PTCA guide wire the Export Aspiration thrombosuction Catheter (Figure 2) was positioned in the ostium of LAD and with maintained negative suction this was advanced distally. After thrombosuction LAD was cleared of any visible thrombus and TIMI – III blood flow was achieved (Figure 3). No stenosis was seen after thrombosuction. Stenting was not required.
Post-Procedure Course in the Hospital:
After Cath-Lab procedure the patient was shifted back to coronary care unit. Intravenous abciximab was continued for next 12 hours. With supportive treatments patient was stabilized, gradually he was weaned off from ventilator & IABP support over next four days. ECG after thrombosuction showed ST segment depression in V1 – V4 with restoration of normal sinus rhythm.
Patient was a non diabetic, normotensive, non smoker. His serum homocysteine level was 46μmol/litre. Blood levels of protein C, protein S, anti-thrombin III, factor V, factor VIII, vWF, fibrinogen, lupus anticoagulant were all within normal limits.
Follow-up Coronary Angiography:
Coronary angiography was repeated (Figure4)after one and a half months which showed absolutely normal coronaries
|
Primary angioplasty and stenting of the occluded culprit artery is now the most widely accepted treatment of acute MI. Dilatation of the coronary artery leads to disruption of plaque and stent-deployment results in shifting of the plaque. Disruption and shifting of plaque may result in distal embolisation of plaque debris or thrombus in an already thrombotic milieu compromising the prospect of effective myocardial salvage. Situation becomes more critical if the infarct related artery is loaded with thrombus.
To overcome this problem different devices have been invented. The Guard Wire Plus System (Percu Surge) distal protection device is an example of such device. Initially Guard Wire Plus System was used in saphenous vein and carotid vessels for containment of embolisation and later it was thought that it can be used in coronary artery. However the experience with this device in coronary artery was not smooth because of long time required in addition to the technical limitations like high profile, need of occlusive mechanism, low trackability and low maneuverability of the device. Still later EAC, (5.4x3.5 Fr distal 35 cm monorail section and 4.6Fr proximal section,135 cm long catheter with0.040 inch diameter of internal lumen that can accommodate 0.014 inch coronary angioplasty guide wire) which is only a component of the Guard Wire Plus System, was designed for thrombosuction.
Woong Chol Kang et al in their series of 62 patients compared PCI plus thrombosuction (Group A-n=31) with PCI minus thrombosuction 2. TIMI flow improved in group A just by performing thrombosuction in 19 patients(61.3%).
Interestingly after thrombosuction with EAC in one patient the coronary flow was completely restored without any distal embolisation or residual stenosis. Thus the procedure was completed without any additional intervention.
The relatively young age and the malignant progression of the ACS in this patient is a typical example of CAD in the Asian Indians3.Hyperhomocysteinaemia was found to be associated as is described in the literature4.
Conclusion: In acute MI thrombosuction with Export Aspiration Catheter can effectively reduce thrombus load of infarct related artery. It may at times be all that is required without any further need of angioplasty & stenting. When post thrombosuction angiographic image demonstrates critical flow-limiting stenotic lesions suitable for angioplasty-stenting, then also thrombosuction prevents or reduces MACE, opening the horizon of successful intervention and reduction in the nightmares of the operator.
References:
1. Global Use Of Strategies To Open Occluded Coronary Arteries in Acute Coronary Syndromes(GUSTO IIb) Angioplasty substudy investigators. A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator in acute MI. N. Engl J Med 1997;336:1621-1628
2. Woong Chol Kang, Tae Hoon Ahn, Seung Hwan Han et al: Thrombosuction utilizing an EAC during PCI in AMI; Yonsei Med J:2007 April;48(2):261-269
3. Enas A. Enas: High rates of CAD in Asian Indians in the United States despite intense modification of life style: what next? Current Science, vol. 74. No. 12, 25th June, 1998
4. Kurt J. Greenlund, Sathanur R. Srinivasan, Ji-Hua Xu: Circulation; 99:2144-2199
|