THE CURRENT STATE OF BETA BLOCKERS IN HYPERTENSION THERAPY.
JOEL A. LARDIZABAL, Prakash C. Deedwania
Division of Cardiology, University of California in San Francisco School of Medicine,
Fresno Medical Education Program
Fresno, CA
Professor of Medicine,University of California in San Francisco School of Medicine
Chief of Cardiology, Veterans Affairs Medical Center in Fresno,
Fresno, CA
|
|
Introduction and Background
For a long time, beta adrenergic blocking agents have been at the frontline in the treatment of hypertension. These agents were considered as first-line antihypertensive therapy for the first time in 1984 when the third report of the Joint National Committee (JNC) on Prevention, Detection, Evaluation and Treatment of High Blood Pressure recommended that beta blockers be an initial therapy option for hypertension, along with thiazide diuretics . With increasing, albeit inconsistent, data as to their efficacy, beta blockers were designated as the “preferred” initial antihypertensive therapy in the JNC-5 report published in 1993 . The designation as a preferred agent was consequently dropped in the JNC-6 report of 1997 , although beta blockers, along with thiazide diuretics, remained the initial therapeutic options in uncomplicated hypertension. The use of beta blockers was also highly advocated in the presence of myocardial infarction as a “compelling indication”. In the subsequent JNC-7 guidelines of 2003, the compelling indications were further expanded to include heart failure, high coronary disease risk, and diabetes .
The Cardioprotective Effects of Beta Blockers
Beta blockers have well-documented anti-ischemic, anti-arryhthmic, anti-atherogenic, neurohormonal system-modulating, and reverse-remodeling properties that make them ideal agents in the presence of these compelling indications .
In the setting of ischemic heart disease, metoprolol, in the Metoprolol in Acute Myocardial Infarction (MIAMI) trial , and atenolol, in the First International Study of Infarct Survival (ISIS-1 trial ), were both associated with a 13-15% reduction in cardiovascular mortality. Even in the era of reperfusion therapy, the Clopidogrel and Metoprolol in Myocardial Infarction Trial (COMMIT) showed that metoprolol, when given in acute myocardial infarction, was associated with 18% reduction in reinfarction and 17% reduction in ventricular arrhythmias . In patients with myocardial infarction complicated by left-ventricular systolic dysfunction, the Carvedilol Post-Infarct Survival Control in LV Dysfunction (CAPRICORN) trial showed that carvedilol reduced the all-cause mortality by 33%, a benefit that is in addition to those of evidence-based treatments, including ACE inhibitors. Cardiovascular mortality and non-fatal myocardial infarctions were also lower on carvedilol compared with placebo . A metaanalysis of trials on patients who sustained myocardial infarction found a 4% acute and 23% long-term mortality reduction with beta blocker therapy .
E-mail: pdeedwania@fresno.ucsf.edu
Telephone: (559) 228-5325
Fax: (559) 228-6961
|
7 This study conclusively demonstrated that rt-PA, a fibrin-selective molecule, was superior to SK, a non–fibrin selective agent, for both early and 1-year mortality reduction. The angiographic sub-study of GUSTO also demonstrated an important relationship between the establishment of early coronary patency and survival. Further modification of the 90-minute front-loaded rt-PA infusions has also been evaluated. Because of superior patency rates with a double-bolus administration of rt-PA 30 minutes apart, this approach was compared with conventional accelerated rt-PA over 90 minutes. Mortality and intracranial hemorrhage tended to be higher with the double-bolus approach, leading investigators to conclude that this modification could not be recommended for general use
Mutants and Variants of rt-PA
r-PA (single-chain nonglycosylated deletion variant of t-pA)
The Recombinant Plasminogen Activator Angiographic Phase II International Dose Finding Study (RAPID) I trial showed that r-PA, when given as a double bolus of 10+10x106 U 30 minutes apart, achieves more rapid, complete, and sustained thrombolysis than standard-dose alteplase (100 mg over 3 hours) 8 In the RAPID II trial, the same r-PA dose regimen yielded 90-minute reperfusion rates that were higher than those of front-loaded rt-PA (59.9% versus 45.2%, P=0.01).9 These promising angiographic findings notwithstanding, r-PA did not achieve superior mortality or clinical outcomes compared with SK (1.5x106 U over 60 minutes) in the International Joint Efficacy Comparison of Thrombolytics (INJECT) study In the GUSTO III trial, which hypothesized the superiority of r-PA over rt-PA, no difference was demonstrated between these agents in 30-day mortality, hemorrhagic stroke, bleeding complications, and the combined end point of death and stroke.
TNK-tPA
Another significant tPA variant is the triple-substitution mutant tenecteplase (TNK-tPA) has a substantially lower plasma clearance rate. In addition, it has higher fibrin selectivity and resistance to inhibition by plasminogen activator inhibitor-1 (PAI-1). 10 In phase 2 studies of TNK-tPA, comparable TIMI 3 patency rates to accelerated rt-PA were demonstrated at 90 minutes.
In patients with chronic ischemia, the Total Ischaemic Burden Bisoprolol Study (TIBBS trial) demonstrated that bisoprolol was superior to the calcium channel blocker (CCB) nifedipine in improving angina and cardiovascular outcomes . Beta blockers were also shown to slow the progression of atherosclerosis in patients with coronary artery disease . Beta blockers reduce inflammation, arterial wall stress, endothelial dysfunction and the risk for plaque rupture. These anti-atherogenic properties may be of particular benefit to patients with diabetes .
In heart failure, the Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF) showed a highly-significant 34% survival advantage in patients treated with long-acting metoprolol compared to placebo . An identical 34% survival benefit was found with bisoprolol therapy in the Cardiac Insufficiency Bisoprolol Study (CIBIS) . This mortality reduction was consistent, whether the etiology of heart failure was ischemic or non-ischemic . There is also data which suggest that initiating heart failure therapy with bisoprolol may be as effective as starting treatment with angiotensin-converting enzyme (ACE) inhibitors . In patients with severe heart failure, treatment with carvedilol was found to be associated with a 35% mortality reduction compared to placebo in the Carvedilol Prospective Randomized Cumulative Survival (COPERNICUS) trial 55.
The anti-arrhythmic efficacy of beta blockers is well-established. In hypertensive men, the Metoprolol Atherosclerosis Prevention in Hypertensives (MAPHY) trial found that metoprolol was associated with 30% reduction in sudden cardiac death . In post-myocardial infarction patients, beta blocker therapy was associated with a 30-50% reduction in sudden cardiac death . In those with heart failure, beta blockers were found to have a more pronounced and more consistent reduction in sudden cardiac death than any other therapy, including ACE inhibitors. The CIBIS-II trial demostrated that bisoprolol reduced sudden cardiac death by 44%, while long-acting metoprolol showed a similar 43% reduction in the MERIT-HF trial .
Doubts Regarding Efficacy of Beta Blockers in Hypertension
Although beta blocker therapy remains indispensable in the presence of compelling indications, a number of studies that emerged shortly after publication of the JNC-7 guidelines have challenged the role of beta blockers as first-line agents in uncomplicated hypertension. In the LIFE trial, the angiotensin receptor blocker (ARB) losartan was shown to be 19% more effective in preventing cardiovascular morbidity and death than the beta blocker atenolol, independent of blood pressure reduction . The Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) also found that atenolol-based antihypertensive therapy was associated with higher rates of cardiovascular events and new-onset diabetes compared with a regimen based on the CCB amlodipine .
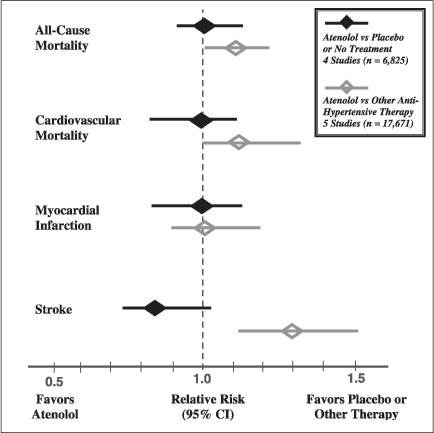
The results of these trials led some investigators to reevaluate the findings from previous beta blocker trials in hypertension. A meta-analysis of 13 randomized controlled trials on hypertension involving over 105,000 patients showed that patients on beta blockers had higher adverse cardiovascular and stroke rates despite similar blood pressure reduction compared with the other classes of agents . A similar meta-analysis of 13 trials involving over 90,000 subjects also found that traditional beta blockers significantly increased the risk of stroke by 24% compared with CCBs, and by 30% compared with angiotensin-converting enzyme (ACE) inhibitors and ARBs . Although beta blocker use significantly reduced stroke and cardiovascular event rates in these studies when compared with placebo or no treatment, such effect was clearly suboptimal when compared to other classes of agents (see Figure 1).
Figure 1. Atenolol Use and Primary Outcomes in Hypertension Trials |
 |
Amidst the scrutiny, the relevance of beta blocker therapy in hypertension treatment was put in serious question. The first official change in treatment policies were made in 2006, when the British guidelines on hypertension were revised, such that beta-blockers were no longer preferred as a routine initial therapy for hypertension, and were moved to fourth step in the treatment of patients with uncomplicated hypertension .
|
Reasons for the Apparent Inefficacy
Several explanations have been proposed for the purported inefficacy of beta blockers in hypertension therapy. Overall, beta blockers were not perceived to be as potent in lowering blood pressure as the other classes of antihypertensive agents. In the the Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) study, treatment with losartan resulted in a 2 mmHg greater reduction in mean systolic blood pressure (SBP) compared with atenolol, and less than half of the patients on beta blocker therapy achieved blood pressure control . In the ASCOT trial, an amlodipine-based regimen was associated with a 1.7 mmHg greater reduction in mean SBP and a 2.0 mmHg lower mean diastolic blood pressure (DBP) compared with atenolol-based therapy, although no link between the magnitude of blood pressure difference and event rates was noted . In a metanalysis of trials involving over 16,000 elderly patients with hypertension, less than one-third of subjects achieved adequate blood pressure control on beta blocker monotherapy, compared to over two-thirds in those treated with diuretics. As a result, beta blocker monotherapy was significantly less effective in preventing coronary heart disease, cardiovascular mortality, and all-cause mortality .
Central aortic pressure has been suggested as a stronger predictor of cardiovascular events than brachial artery blood pressure. The Conduit Artery Function Evaluation (CAFÉ) substudy of the ASCOT trial showed that despite similar reduction in peripheral blood pressure, atenolol-based therapy was associated with 4.3 mmHg higher central aortic systolic blood pressure and 3 mmHg central aortic pulse pressure measurements when compared to amlodipine. This was felt to contribute to the 14% higher risk of coronary events and 23% higher stroke risk in the atenolol-treated patients .
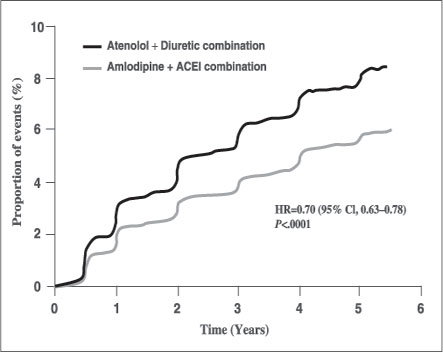
In addition to the apparent suboptimal antihypertensive efficacy, multiple studies have also shown that beta blocker therapy has adverse metabolic effects, and could lead to the development of diabetes and dyslipidemia. In the Atherosclerosis Risk in Communities (ARIC) Study, patients with hypertension who were taking beta blockers had a 28% higher risk of subsequent diabetes compared to those not on any therapy. Those taking other antihypertensive classes of agents, including thiazides, did not appear to increase diabetes risk . The LIFE study revealed that atenolol was associated with a 31% increased risk of new-onset diabetes compared with losartan6. Similarly in the ASCOT trial, atenolol therapy was linked to a 30% higher risk of incident diabetes compared with amlodipine7 (see Figure 2). A metaanalysis of 12 trials involving 94,492 patients taking beta blockers (predominantly atenolol) as first-line therapy for hypertension found a 22% increased risk for new-onset diabetes. This risk increased exponentially with increased duration of beta blocker treatment .
Beta blockers could potentially increase insulin resistance and promote incident diabetes by attenuating beta-receptor mediated insulin release from pancreatic beta cells, decreasing microvascular flow in skeletal muscle, and inducing weight gain16.
| Figure 2. Risk of New-Onset Diabetes with Atenolol-Based Therapy (Reproduced from Dahlöf B, et al. Lancet. 2005;366:895-906.) |
 |
Chronic beta blocker therapy may also decrease high-density lipoprotein (HDL) cholesterol up to 20% and increase triglyceride levels up to 50%, especially with nonselective agents without intrinsic sympathomimetic activity. It is theorized that unopposed alpha-adrenergic stimulation as a result of suppression of beta-adrenergic activity causes increased inhibition of lipoprotein lipase activity, which in turn decreases catabolism of triglycerides and increases catabolism of HDL .
Further contributing to the inefficacy of beta blockers as first-line antihypertensives is the adverse event profile of these agents that leads to poor compliance. Undesirable side effects are abundant, and include erectile dysfunction, depression, lethargy, drowsiness, hallucinations, nightmares, airway hyperreactivity, peripheral vasoconstriction, among many others. Patients on beta-blockers are 80% more likely to discontinue treatment than those on diuretics, and 41% more likely to withdraw from therapy than those on RAAS blockers .
Not all Beta Blockers are Similar
The vast majority of hypertension trials that involved beta blockers used atenolol as the reference agent. In the metaanalyses22,23 that questioned the role of beta blockers as first-line antihypertensive agents, half of all trials analyzed (representing over 70% of patients studied) used atenolol. Further analysis of these same trials found that non-atenolol beta blockers were actually associated with better cardiovascular outcomes compared to atenolol . It is, therefore, not entirely accurate to label all beta blocking agents as inferior drugs for hypertension therapy based on these studies since atenolol does not appear to be representative of the beta-adrenergic blocker class as a whole.
|
Data on non-atenolol beta blockers (e.g. metoprolol and bisoprolol) show similar or even greater antihypertensive efficacy as other classes of agents, without the adverse metabolic effects , , , . Also, the new-generation vasodilating beta blockers, which possess hemodynamic and metabolic properties different from that of the traditional agents, have not been well-represented in the hypertension trials.
In contrast to other beta blockers, atenolol has a low lipophilic profile making it much less permeable to the central nervous system (the amount of beta blocker in the brain correlates with the drug’s antiarrhythmic potential). Beta-1 selectivity varies among different cardioselective agents, and atenolol was shown to have lower beta-1 and much higher beta-2 antagonistic activities compared to other agents . Lower beta-1 selectivity could explain why atenolol was not as effective as other agents in reducing left ventricle hypertophy , . Atenolol also has some beta-2 blocking activity that might account for its negative metabolic effects, as agents with higher cardioselectivity do not seem associated with adverse effects on glucose and lipid metabolism . In addition, chronic therapy with other beta blockers like metoprolol leads to peripheral vasodilatation, but this has not been demonstrated with atenolol .
Furthermore, atenolol has a half-life of only 6 to 7 hours, but it has been marketed as a once-daily drug. Patients on this therapy are thus exposed to prolonged periods of inadequate or absent beta blockade during treatment. Also, abrupt interruption of beta blocker therapy could lead to a rebound phenomenon that is associated with adverse cardiac outcomes . It is conceivable that these fluctuations in plasma levels of atenolol could potentially induce adverse physiologic responses akin to beta blocker withdrawal syndrome.
Mechanisms for the Antihypertensive Actions of Beta Blockers
There is considerable pharmacologic heterogeneity among beta blockers, and individual agents exert different physiologic effects that are largely dependent on their affinity to particular adrenoreceptors. To date, there are 3 known types of beta adrenergic receptors (β1, β2 and β3), each mediating a different physiologic response. It is presumed that beta blockers reduce both systolic and diastolic pressure in hypertensive patients at rest and during exercise, mostly through their effects on beta-1 adrenoreceptors which are concentrated mainly in the heart and kidneys. Stimulation of cardiac beta-2 adrenoreceptors induces positive chronotropic and inotropic cardiac effects, and antagonism of these receptors attenuates the contractile response to cathecholamines, decreases heart rate, reduces cardiac output, and ultimately lowers blood pressure. Stimulation of these receptors in the macula densa of the kidneys induces renin release. Antagonism by beta blockers, therefore, inhibits renin secretion from the kidneys, leading to downregulation of the angiotensin-aldosterone axis, resulting in reduction in plasma volume, vasomotor tone and peripheral vascular resistance .
Stimulation of beta-2 adrenoreceptors (found mostly in the lungs, gastrointestinal tract, liver, uterus, vascular smooth muscle, and skeletal muscle) results in bronchodilation, smooth muscle relaxation, skeletal muscle tremor and glycogenolysis. Activation of beta-3 receptors, located in fat cells, stimulates lipolysis. The reported metabolic derangements associated with beta blocker therapy (dyslipidemia, dysglycemia, and insulin resistance) stem from antagonism of the beta-2, and possibly beta-3, adrenoreceptors44.
The older, first-generation beta blockers (e.g. propranolol, pindolol, nadolol) are non-selective in that they antagonize all beta-adrenergic receptors. The second-generation agents (e.g. atenolol, metoprolol, bisoprolol, xamoterol) are relatively cardioselective because of higher specificity to beta-1 receptors, although this selectivity is diminished at higher doses44. Combined beta-1 and beta-2 antagonism, by blocking vasodilatory β2- receptors and by permitting unopposed alpha-induced vasocontriction , diminishes antihypertensive activity, making non-selective agents less effective than the cardioselective beta blockers in reducing blood pressure, especially in smokers .
Some agents can show both agonism and antagonism at a particular beta receptor, depending on the concentration of the drug and the concentration of the endogenous cathecholamines. This property, termed “intrinsic sympathomimetic activity” (ISA), theoretically allows these agents to counteract the hazards of random sympathetic stimulation without negatively affecting cardiac output, heart rate or metabolism . Possession of beta-2 ISA (e.g. pindolol) lowers blood pressure through beta-2-mediated vasodilation as well as reduction in plasma norepinephrine levels, without significant effect on heart rate, cardiac output, or renin activity . However, neurohormonal responses to ISA may impair the anti-ischemic and cardioprotective effects of such beta blockers in ischemic heart disease and heart failure .
The newest generation of agents (e.g. carvedilol) exhibits mixed antagonism of both beta and alpha-1 adrenergic receptors, which provides additional arteriolar vasodilating action, hence the term “vasodilating beta blockers”. Alpha-1 adrenergic receptors, found principally in smooth muscle cells, mediate cathecholamine-driven peripheral, central and coronary vasoconstriction. Blockade of alpha-1 receptors attenuates the adrenergic pressor response, promotes vasodilatation, and improves vascular compliance leading to reduction in blood pressure .
|
The Vasodilating Beta Blockers
The advent of the latest-generation vasodilating beta blockers has enjoyed an enthusiastic reception thus far. With improved antihypertensive potency, enhanced hemodynamic profile, better tolerability and reduced adverse metabolic outcomes, these agents are perceived to address the negative effects associated with classical beta blockers, especially with regards to blood pressure-lowering efficacy, insulin resistance, weight gain, and sexual dysfunction.
Carvedilol is a non-cardioselective beta blocker that antagonizes alpha-1, beta-1, and beta-2 adrenergic receptors. Alpha-1 inhibition is responsible for the vasodilatory property of carvedilol, which, in addition to reduction in peripheral vascular resistance, can also improve metabolic parameters, as well as enhance renal blood flow and sodium excretion . As an antihypertensive agent, carvedilol has been shown to have greater reduction in both systolic and diastolic blood pressures compared to metoprolol, a benefit attributed to added vasodilation .
Nebivolol, another vasodilating agent, is highly cardioselective, with beta-1 selectivity that is ten times that of metoprolol and over 2.5 times that of bisoprolol (agents which are highly cardioselective themselves). Its vasodilating property is thought to arise from potentiation of nitric oxide release from and enhanced bioavailability at the endothelium. Treatment with nebivolol causes a 13% reduction in peripheral resistance, along with modest heart rate reduction, effectively reducing blood pressure. There is also a concomitant 20% increase in stroke volume, thereby preserving cardiac output .
Devoid of ISA, these vasodilating agents appear to have less of the undesirable effects of the classic beta blockers. In the COPERNICUS trial, more patients who were taking placebo withdrew because of adverse effects compared with patients who were taking carvedilol . One particular side effect of beta blockers that might contribute to poor compliance to therapy is sexual dysfunction . Traditional beta blockers cause peripheral vasoconstriction which decreases blood flow to the corpora cavernosa, contributing to erectile dysfunction. In male hypertensive patients, nebivolol therapy was associated with improved indices of erectile function, sexual desire, orgasmic function, and intercourse satisfaction compared with metoprolol . Increased nitric oxide availability is the likely mechanism for such effect.
Although concerns have been raised about the dysglycemic effects of beta blockers, it is also recognized that ischemic heart disease and heart failure (for which beta blocker therapy is of proven benefit) are more common in the diabetic than in nondiabetic population. It is thought
that the traditional beta blockers may precipitate or exacerbate diabetes through peripheral vasoconstriction, which reduces the skeletal muscle microvascular surface area for insulin-mediated glucose entry and metabolism, promoting insulin resistance. Presumbaly because of their vasodilating property, carvedilol and nebivolol were found to have better metabolic profile and have desirable effects on insulin sensitivity than other beta blockers, prompting the American Association of Clinical Endocrinologists to state that they may be of particular benefit in hypertensive diabetic patients .
The Glycemic Effects in Diabetes Mellitus: Carvedilol-Metoprolol Comparison in Hypertensives (GEMINI) trial compared the metabolic effects of carvedilol and metoprolol in hypertensive patients with diabetes. This large randomized multicenter study demonstrated that metoprolol significantly increased weight, triglycerides and glycated hemoglobin, while carvedilol has no adverse effects on such parameters . In patients with diabetes, carvedilol was also shown to significantly improve endothelial function compared to metoprolol despite similar effects on blood-pressure . Nebivolol, on the other hand, not only was associated with less worsening of insulin resistance compared to metoprolol, it also significantly reduced insulin resistance compared to baseline .
Although large head-to-head randomized controlled trials on these newer beta blockers are lacking with regards to hypertension, there are data to suggest that these vasodilating agents have similar or even greater cardioprotective effects as traditional beta blockers. Carvedilol, as previously mentioned, was shown in the CAPRICORN trial to significantly reduce mortality and adverse cardiac events in patients with myocardial infarction and systolic dysfunction. Nebivolol, on the other hand, may increase coronary flow reserve and collateral flow in patients with coronary artery disease , although it has yet to be adequately tested in the setting of ischemic heart disease.
Carvedilol is associated with improved survival in the setting of heart failure, and this mortality benefit was shown by the Carvedilol Or Metoprolol European Trial (COMET) to be 17% greater compared to metoprolol, a drug already proven beneficial in heart failure therapy . The experience on nebivolol in heart failure, on the other hand, is limited. In the Study of the Effects of Nebivolol Intervention on Outcomes and Rehospitalisation in Seniors with Heart Failure (SENIORS trial), nebivolol therapy was associated with a modest 14% reduction in the combined outcome of all-cause mortality or cardiovascular hospitalization compared to placebo. However, no difference was seen in either all-cause or cardiovascular mortality .
Clinical Relevance of Beta Blocker Therapy in Hypertension
There is no question that beta blockers are the mainstay of therapy in the setting of ischemic heart disease, heart failure, arrhythmias, and high coronary disease risk. What has become unclear at present is whether or not beta blockers should be considered as preferred agents in uncomplicated hypertension, especially when used alone as monotherapy.
|
Given the preponderance of data pointing towards their relative inefficacy, atenolol and the older non-selective beta blockers probably should no longer be used as first-, second-, or even third-line therapies for uncomplicated hypertension. These drugs also lack the cardioprotective effects of other beta blockers, so they are no longer indicated for the treatment of heart failure and ischemic heart disease as well. The same can be said with beta blockers possessing ISA, which are not cardioprotective and have performed poorly in heart failure trials , .
Agents with higher cardioselectivity should still remain as viable antihypertensive options, either as monotherapy or in combination with other classes. Analysis of the MAPHY substudy of hypertensive patients showed that metoprolol had a similar blood pressure reduction as thiazide diuretics, but was associated with a 24% lower risk for coronary events . Metoprolol also afforded the same hypertension control and renal protection as the ACE inhibitor enalapril on long-term follow-up of patients with primary hypertension . Similar findings were seen with bisoprolol .
In elderly individuals, cardiac risk associated with hypertension is determined predominantly by large artery stiffness and increased peripheral pulse wave reflectance . It is to be expected then that classic beta blockers, which are not known to improve vascular compliance, would be relatively ineffective in older individuals, especially since elderly hypertensives have low beta-receptor sensitivity and low renin activity. A vasodilating beta blocker which increases vascular compliance and has less metabolic side effects would be a reasonable choice in these patients. Both carvedilol and nebivolol have been shown to be effective in the elderly population.
On the other hand, the young and middle-aged hypertensives have high renin and high adrenergic states . These conditions make beta-1 selective beta blockers (e.g. metoprolol, bisoprolol) attractive first-line options for hypertension therapy in young individuals. Most appropriate in these young patients, perhaps, would be nebivolol, which has the highest beta-1 selectivity and has less adverse effects on sexual function.
Sympathetic hyperactivity is also the predominant feature of hypertensive patients with diabetes, and this may be one of the many mechanisms resulting in the greater cardiovascular complications seen in these individuals . The highly-cardioselective or the vasodilating beta blockers, which have lesser effects on glucose metabolism, appear well-suited for these patients.
Conclusion
Beta adrenergic blockers have had a long history of being one of the most prominent classes of drugs in cardiovascular therapeutics. They remain as the mainstay therapy in the setting of ischemic heart disease, heart failure, high coronary disease risk and arrhythmias, as their importance in these compelling indications are well-established. Questions, however, have been raised regarding the efficacy and relevance of beta blockers in the treatment of uncomplicated hypertension because the traditional agents (atenolol, in particular) were deemed not at par with agents from other classes in terms of cardiovascular outcomes. Although atenolol and other traditional agents have lost favor, the other cardioselective agents have been shown to be at least as efficacious in hypertension as the other classes of drugs. Their use in hypertension therapy should continue, especially in young and diabetic individuals where high sympathetic tone and high renin levels are the primary features. The newer-generation vasodilating beta blockers have favorable hemodynamic and metabolic profiles, better side effect background, and improved efficacy in treating uncomplicated hypertension. With the advent of these new agents, the beta blocker class should remain as a viable first-line option in antihypertensive therapy.
1. Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The 1984 Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1984;144:1045–1057.
2. Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. The Fifth Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure (JNC V). Arch Intern Med. 1993;153:154–183.
3. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997;157:2413–2446.
4. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003 Dec;42(6):1206-52.
5. Fonarow GC. Managing the patient with diabetes mellitus and heart failure: issues and considerations. Am J Med. 2004;116:76-88S.
6. The MIAMI Trial Research Group. Metoprolol in acute myocardial infarction (MIAMI). A randomised placebo-controlled international trial. Eur Heart J. 1985;6(3):199-226.
7. First International Study of Infarct Survival Collaborative Group. Randomised trial of intravenous atenolol among 16 027 cases of suspected acute myocardial infarction: ISIS-1. Lancet. 1986;2(8498):57-66.
8. COMMIT (ClOpidogrel and Metoprolol in Myocardial Infarction Trial) collaborative group. Early intravenous then oral metoprolol in 45,852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet. 2005;366(9497):1622-32.
9. Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001;357(9266):1385-90.
10. Freemantle N, Cleland J, Young P, Mason J, Harrison J. Beta Blockade after myocardial infarction: systematic review and meta regression analysis. BMJ. 1999;318(7200):1730-7.
11. von Arnim T. Medical treatment to reduce total ischaemic burden: total ischaemic burden bisoprolol study (TIBBS), amulticentre trial comparing bisoprolol and nifedepine. J Am Coll Cardiol 1995;25:231–8.
12. Sipahi I, Tuzcu EM, Wolski KE, Nicholls SJ, Schoenhagen P, Hu B, et al. Beta-blockers and progression of coronary atherosclerosis: pooled analysis of 4 intravascular ultrasonography trials. Ann Intern Med. 2007;147(1):10-8.
13. Tse WY, Kendall M. Is there a role for beta-blockers in hypertensive diabetic patients? Diabet Med. 1994;11(2):137-44.
14. MERIT-HF Investigators. Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet. 1999;353(9169):2001-7.
15. CIBIS-II Investigators. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet. 1999;353(9146):9-13.
16. Fauchier L, Pierre B, de Labriolle A, Babuty D. Comparison of the beneficial effect of beta-blockers on mortality in patients with ischaemic or non-ischaemic systolic heart failure: a meta-analysis of randomised controlled trials. Eur J Heart Fail. 2007;9(11):1136-9.
17. CIBIS III Investigators. Effect on survival and hospitalization of initiating treatment for chronic heart failure with bisoprolol followed by enalapril, as compared with the opposite sequence: results of the randomized Cardiac Insufficiency Bisoprolol Study (CIBIS) III. Circulation. 2005;112(16):2426-35.
18. Olsson G, Tuomilehto J, Berglund G, Elmfeldt D, Warnold I, Barber H, et al. Primary prevention of sudden cardiovascular death in hypertensive patients. Mortality results from the MAPHY study. Am J Hypertens. 1991; 4:151-8.
19. Kendall MJ, Lynch KP, Hjalmarson A, Kjekshus J. Beta-blockers and sudden cardiac death. Ann Intern Med. 1995 Sep 1;123(5):358-67.
20. Domanski MJ, Krause-Steinrauf H, Massie BM, Deedwania P, et al. A comparative analysis of the results from 4 trials of beta-blocker therapy for heart failure: BEST, CIBIS-II, MERIT-HF, and COPERNICUS. J Card Fail. 2003 Oct;9(5):354-63.
|
22. Dahlöf B, Sever PS, Poulter NR, et al; ASCOT Investigators. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet. 2005 Sep 10-16;366(9489):895-906.
23. Lindholm LH, Carlberg B, Samuelsson O. Should beta blockers remain first choice in the treatment of primary hypertension? A meta-analysis. Lancet. 2005;366:1545-1553.
24. Bradley H, Wiysonge C, Volmink J, Mayosi B, Opie L. How strong is the evidence for use of beta-blockers as first-line therapy for hypertension? Systematic review and meta-analysis. Journal of Hypertension, 2006; 24:2131-2141.
25. BHS/NICE. Hypertension: management of hypertension in adults in primary care. June 2006. http://www.nice.org.uk/CG034guidance#summary.
26. Lindholm LH, Ibsen H, Dahlöf B, et al; LIFE Study Group. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002 Mar 23;359(9311):1004-10.
27. Poulter NR, Wedel H, Dahlöf B, et al; ASCOT Investigators. Role of blood pressure and other variables in the differential cardiovascular event rates noted in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA). Lancet. 2005 Sep 10-16;366(9489):907-13.
28. Messerli FH, Grossman E, Goldbourt U. Are beta-blockers efficacious as first-line therapy for hypertension in the elderly? A systematic review. JAMA. 1998 Jun 17;279(23):1903-7.
29. The CAFE Investigators, for the Anglo-Scandinavian Cardiac Outcomes Trial (ASCOT) Investigators. Differential Impact of Blood Pressure–Lowering Drugs on Central Aortic Pressure and Clinical Outcomes: Principal Results of the Conduit Artery Function Evaluation (CAFE) Study. Circulation. 2006;113:1213-1225.
30. Gress TW, Nieto FJ, Shahar E, Wofford MR, Brancati FL. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus: Atherosclerosis Risk in Communities Study. N Engl J Med. 2000 Mar 30;342(13):905-12.
31. Bangalore S, Parkar S, Grossman E, Messerli FH. A meta-analysis of 94,492 patients with hypertension treated with beta blockers to determine the risk of new-onset diabetes mellitus. Am J Cardiol. 2007 Oct 15;100(8):1254-62.
32. Weir MR, Moser M. Diuretics and beta-blockers: is there a risk for dyslipidemia? Am Heart J. 2000 Jan;139(1 Pt 1):174-83.
33. Bradley HA, Wiysonge CS, Volmink JA, Mayosi BM, Opie LH. How strong is the evidence for use of beta-blockers as first-line therapy for hypertension? Systematic review and meta-analysis. J Hypertens. 2006 Nov;24(11):2131-41.
34. Aursnes I, Osnes J, Tvete I, Gåsemyr J, NatvigB. Does atenolol differ from other β-adrenergic blockers? BMC Clin Pharm. 2007;7:4.
35. Wikstrand J, Warnold I, Tuomilehto J, Olsson G, Barber HJ, Eliasson K, et al. Metoprolol versus thiazide diuretics in hypertension: morbidity results from the MAPHY Study. Hypertension. 1991;17(4):579-88.
36. Aurell M, Bengtsson C, Björck S. Enalapril versus metoprolol in primary hypertension--effects on the glomerular filtration rate. Nephrol Dial Transplant. 1997;12(11):2289-94.
37. Bracchetti D, Gradnik R, Alberti A, et al. A double-blind comparison of bisoprolol and captopril for treatment of essential hypertension in the elderly. Cardiovasc Drugs Ther. 1990 Feb;4(1):261-4.
38. Bueno J, Amiguet JA, Carasusan J, Cebollada J, Carretero J. Bisoprolol vs. chlorthalidone: a randomized, double-blind, comparative study in arterial hypertension. J Cardiovasc Pharmacol. 1990;16 Suppl 5:S189-92.
39. Nuttall SL, Routledge HC, Kendall MJ. A comparison of the beta1-selectivity of three beta1-selective beta-blockers. J Clin Pharm Ther. 2003;28(3):179-86.
40. Gosse P, Roudaut R, Herrero G, Dallocchio M. Beta-blockers vs. angiotensin-converting enzyme inhibitors in hypertension: effects on left ventricular hypertrophy. J Cardiovasc Pharmacol. 1990;16 Suppl 5:S145-50.
41. Agabiti-Rosei E, Ambrosioni E, Dal Palù C, Muiesan ML, Zanchetti A. ACE inhibitor ramipril is more effective than the beta-blocker atenolol in reducing left ventricular mass in hypertension. Results of the RACE (ramipril cardioprotective evaluation) study on behalf of the RACE study group. J Hypertens. 1995;13(11):1325-34.
42. Saku K, Liu K, Takeda Y, Jimi S, Arakawa K. Effects of lisinopril and bisoprolol on lipoprotein metabolism in patients with mild-to-moderate essential hypertension. Clin Ther. 1995 Nov-Dec;17(6):1136-46.
43. Christensen KL, Mulvany MJ. Vasodilatation, not hypotension, improves resistance vessel design during treatment of essential hypertension: a literature survey. J Hypertension. 2001;19:1001-6.
44. Frischman WH. Beta-adrenergic blocker withdrawal. Am J Cardiol. 1987; 59:26F–32F.
45. Waller D. Beta-adrenoceptor partial agonists: a renaissance in cardiovascular therapy? Br J Clin Pharmacol. 1990; 30(2):157–171.
46. Trap-Jensen J, Carlsen JE, Svendsen TL, Christensen NJ. Cardiovascular and adrenergic effects of cigarette smoking during immediate non-selective and selective beta adrenoceptor blockade in humans. Eur J Clin Invest. 1979;9(3):181-3.
47. Prichard BN, Cruickshank JM, Graham BR. Beta-adrenergic blocking drugs in the treatment of hypertension. Blood Press. 2001;10(5-6):366-86.
48. Taylor SH. Intrinsic sympathomimetic activity: clinical fact or fiction? Am J Cardiol. 1983 Nov 10;52(9):16D-26D.
49. Man in 't Veld AJ, Schalekamp MA. Effects of 10 different beta-adrenoceptor antagonists on hemodynamics, plasma renin activity, and plasma norepinephrine in hypertension: the key role of vascular resistance changes in relation to partial agonist activity. J Cardiovasc Pharmacol. 1983;5 Suppl 1:S30-45.
50. Van Den Heuvel AF, van der Ent M, van Veldhuisen DJ, Kruijssen DA, Bartels GL, Remme WJ. Effects of epanolol, a selective beta1-blocker with intrinsic sympathomimetic activity, in patients with ischemic left ventricular dysfunction. J Cardiovasc Pharmacol. 1998;31(4):506-12.
51. van Zwieten PA. An overview of the pharmacodynamic properties and therapeutic potential of combined alpha- and beta-adrenoceptor antagonists. Drugs. 1993;45(4):509-17.
52. Bakris GL, Hart P, Ritz E. Beta blockers in the management of chronic kidney disease. Kidney Int. 2006;70(11):1905-13.
53. Weber K, Bohmeke T, van der Does R, Taylor SH. Comparison of the hemodynamic effects of metoprolol and carvedilol in hypertensive patients. Cardiovasc Drugs Ther. 1996;10(2):113-7.
54. Kamp O, Sieswerda GT, Visser CA. Comparison of effects on systolic and diastolic left ventricular function of nebivolol versus atenolol in patients with uncomplicated essential hypertension. Am J Cardiol. 2003;92:344-348.
55. Carvedilol Prospective Randomized Cumulative Survival Study Group. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001;344(22):1651-8.
56. Wassertheil-Smoller S, Blaufox MD, Oberman A, et al. Effect of antihypertensives on sexual function and quality of life: the TAIM Study. Ann Intern Med. 1991;114(8):613-20..
57. Brixius K, Middeke M, Lichtenthal A, Jahn E, Schwinger RH. Nitric oxide, erectile dysfunction and beta-blocker treatment (MR NOED study): benefit of nebivolol versus metoprolol in hypertensive men. Clin Exper Pharmacol Phys. 2007;34:327-331.
58. AACE Hypertension Task Force. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the diagnosis and treatment of hypertension. Endocr Pract. 2006;12(2):193-222.
59. GEMINI Investigators. Metabolic effects of carvedilol vs metoprolol in patients with type 2 diabetes mellitus and hypertension: a randomized controlled trial. JAMA. 2004;292(18):2227-36.
60. Bank AJ, Kelly AS, Thelen AM, Kaiser DR, Gonzalez-Campoy JM. Effects of carvedilol versus metoprolol on endothelial function and oxidative stress in patients with type 2 diabetes mellitus. Am J Hypertens. 2007;20(7):777-83.
61. Celik T, Iyisoy A, Kursaklioglu H, et al. Comparative effects of nebivolol and metoprolol on oxidative stress, insulin resistance, plasma adiponectin and soluble P-selectin levels in hypertensive patients. J Hypertens. 2006;24:591-596.
62. Togni M, Vigorito F, Windecker S, et al. Does the beta-blocker nebivolol increase coronary flow reserve? Cardiovasc Drugs Ther. 2007;21(2):99-108.
63. Carvedilol Or Metoprolol European Trial Investigators. Comparison of carvedilol and metoprolol on clinical outcomes in patients with chronic heart failure in the Carvedilol Or Metoprolol European Trial (COMET): randomised controlled trial. Lancet. 2003 Jul 5;362(9377):7-13.
64. SENIORS Investigators. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005;26(3):215-25.
65. Xamoterol in Severe Heart Failure Study Group. Xamoterol in severe heart failure. Lancet 1990;336:1–6.
66. The Beta-blocker Evaluation of Survival Trial Investigators. A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N Eng J Med 2001;344:1659–67.
67. Wikstrand J, Warnold I, Tuomilehto J, Olsson G, Barber HJ, Eliasson K, et al. Metoprolol versus thiazide diuretics in hypertension: morbidity results from the MAPHY Study. Hypertension. 1991;17(4):579-88.
68. Aurell M, Bengtsson C, Björck S. Enalapril versus metoprolol in primary hypertension--effects on the glomerular filtration rate. Nephrol Dial Transplant. 1997;12(11):2289-94.
69. Johns TE, Lopez LM. Bisoprolol: is this just another beta-blocker for hypertension or angina? Ann Pharmacother. 1995;29(4):403-14.
70. Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circulation 2001;103:1245–9.
71. Feldman RD, Limbird LE, Nadeau J, Robertson D, Wood AJJ. Alterations in leucocyte beta-receptor affinity with ageing. N Engl J Med 1984;310:815–9.
72. Morgan TO, Anderson A, Cripps J, Adam W. The use of carvedilol in elderly hypertensive patients. Eur J Clin Pharmacol. 1990;38 Suppl 2:S129-33.
73. Mazza A, Gil-Extremera B, Maldonato A, Toutouzas T, Pessina AC. Nebivolol vs amlodipine as first-line treatment of essential arterial hypertension in the elderly. Blood Press. 2002;11(3):182-8.
74. Bühler FR, Burkart F, Lütold BE, Küng M, Marbet G, Pfisterer M. Antihypertensive beta blocking action as related to renin and age: a pharmacologic tool to identify pathogenetic mechanisms in essential hypertension. Am J Cardiol. 1975;36(5):653-69.
75. Palatini P, Longo D, Zaetta V, Perkivic D, Garbelotto R, Pessina AC. Evolution of blood pressure and cholesterol in stage 1 hypertension: role of autonomic nervous system activity. J Hypertens 2006;24:1375–81.
76. Huggett RJ, Scott EM, Gilbey SG, Stoker JB, Mackintosh AF, Mary DA. Impact of type 2 diabetes mellitus on sympathetic neural mechanisms in hypertension. Circulation. 2003;108(25):3097-101.
|