Coronary Vasospasm Presenting As Prinzmetals Angina and Life
Threatening Brady-arrhythmia Independently at Different Times
Aijaz H Mansoor, Praveer Aggarwal, Sanjeev Bhardwaj,
Vivek Tandon, Upendra Kaul
Department of Cardiology, Escorts heart institute and research centre,New Delhi
|
|
INTRODUCTION
‘Variant Angina’ was first described by Prinzmetal (1). It is characterized by episodes of chest pain at rest, associated with ST segmental elevation in the ECG. It mostly occurs in early morning hours, often in clusters, that last for 3 to 6 months, before abating. The underlying coronary anatomy is variable. A lower incidence of fixed atherosclerotic lesions has been noted in Japanese patients as compared to western patients.(2).
The mechanism is vasospasm is unclear. Factors implicated include endothelial dysfunction and activation of the autonomic nervous system.
We hereby present an unusual case of coronary vasospasm presenting as recurrent episodes of variant angina and recurrent symptomatic complete heart block and asystole occurring independent of each other at different times.
Case Report:
A 65 yrs old lady presented to us with a history of retrosternal chest pain and recurrent vomiting of 4 days duration. Four days before being seen by us she had episodes of unprovoked chest pain at rest, associated with vomiting and sweating, lasting 10-20 minutes. There was no concurrent dyspnea and the pain had no relation to posture or respiration.
She reported to her local hospital, where she was found to have severe hypertension (250/130mmhg.). Her initial ECG was regarded as normal and spot trop T was negative.
Subsequent qualitative Trop T was found positive. She was admitted and managed as NSTEMI with accelerated hypertension. She received aspirin 150 mgs, clopidogrel 75 mgs, enoxaparin (1mg/kg twice a day), and nitroglycerine and atorvastatin 40 mgs. She became asymptomatic. 2 days later she had an episode of sudden dizziness in the early morning hours, while in the hospital. No chest pain was reported. The ECG recorded compete heart block with a wide QRS, slow escape rhythm (Fig 1 ). She received atropine 2 ampoules I/V and sinus rhythm was restored. There were no accompanying ST T Changes. Two days later, she had recurrence of chest heaviness with hypotension. She received I/V fluids, and was referred to our institute for further management. Except for hypertension and history of cholecystectomy.10 years ago, her past history was unremarkable. She was a non smoker, with no family history of premature coronary artery disease or sudden cardiac death.
On examination, she was conscious, and comfortable. Pulse was 88 bpm and regular, blood pressure was 150/70 mm hg .The clinical examination was unremarkable. ECG showed normal sinus rhythm with no ST –T changes.(fig 2). The chest X ray was unremarkable. Echocardiography and Doppler examination revealed a normal LV, normal valves and no pericardial effusion. A Complete blood count, urine analysis, blood chemistries (Kidney function, liver function, blood sugar) and electrolytes were within normal limits. CK, CK–MB were in the normal range, but Trop T was elevated at 0.25 ng/ml. She was treated with intravenous nitroglycerine infusion, enoxaparin and statins. Non dihydropyridine calcium blockers ( diltizem) were initiated.
 |
 |
Fig 1. Patient in complete heart block (upper panel). Atropine I/V was administered as this ECG was being recorded. The precordial leads (lower panel) show atropine-induced sinus tachycardia. |
Correspondence : Prof. Upendra Kaul, Executive Director, Department of Cardiology, Escorts Heart Institute & Research Centre, Okhla Road,
New Delhi – 110 025
Phone No. 91-11-26825000, Email : ukaul@vsnl.com
|
Next morning at 4 am, she again had sudden dizziness, without chest pain and was found to have CHB with a heart rate of 30 bpm (wide QRS, slow escape rhythm). This was followed rapidly by asystole. She received immediate cardiac massage and 2mg of i/v atropine. She reverted to
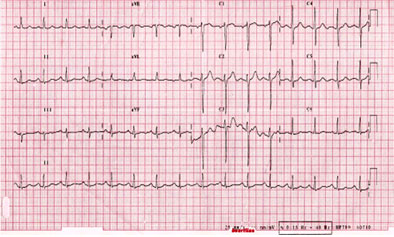 |
| Fig 2. ECG on presentation to our hospital. Normal sinus rhythm and no ischaemic ST-T changes. |
sinus rhythm without any ST – T changes. A temporary pacemaker was inserted, and her condition stabilized. At 8:44am same morning she complained of severe chest pain and sweating. ECG revealed ST elevatation in inferior leads and V6 without any AV block. (Figure 3) In a few minutes her pain subsided, and repeat ECG showed normal sinus rhythm with normalization of ST segments. She was shifted to Cardiac catheterization lab for urgent coronary angiography. The angiography revealed multiple sites of narrowing in left anterior descending artery, circumflex and right coronary arteries (fig 4). Intra coronary nitroglycerine relieved these obstructions (Figure 5). Her coronaries after intra coronary NTG looked entirely normal. The AV nodal branch had no disease and was flowing briskly. She remained in normal sinus rhythm during and after the procedure.
She underwent an electrophysiologic study next day which was normal with no evidence of sinus node, AV node or infra or intra-Hisian disease. SVT or VT could not be induced. The study was done after stopping nitroglycerine and was repeated while on nitroglycerine. Ergonovine provocation was not done for fear of precipitating coronary vasospasm which had already been demonstrated. However same evening she again complained of dizziness without chest pain and ECG evidence of transient complete heart block. in absence of ST T changes either before or during the episode.
 |
||
| Fig 3. ECG during painful vasospasm. Acute ST elevation seen in inferior leads. | ||
|
||
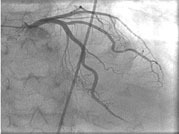
| Fig 4. Coronary Angiogram before the administration of intracoronary nitroglycerine. Diffuse and multiple sites of focal narrowing seen in right as well as in left coronary arteries (arrows). | ||
|
||
| Fig 5. Coronary Angiogram after intra-coronary nitroglycerine. Relief of spasm and normal coronary arteries seen. | ||
|
Discussion:
Variant angina is more frequently seen in East Asia as compared to West. 2-3 % of all patients undergoing coronary angiography for chest pain in the USA, are assigned a diagnosis of Varient angina, as against 20-30% in Japan (3) The condition is not common in our setting and incidence has not been reported, though there are anecdotal case reports.
It is mainly seen in younger females, who usually have no risk factors, except smoking. The chest pain is usually unprovoked. It can be precipitated by alcohol, nicotine, ergonovine, acetylcholine, hyperventilation, REM sleep, drinking iced drinks and atrial pacing.The attacks can be prevented or reverted by atropine, alfa receptor blockers (Prazosin) and calcium channel blockers of both dihydropyridine (nifedipine) and non dihydropyridine class (verapamil and diltiazem).
Our patient had very unusual features besides being elderly without a past history.. The presentation had peculiarities that the chest pain and ST elevation in inferior leads was present without heart block. The heart block and asystole was seen in episodes of dizziness without ST changes in ECG or chest pain. The episodes of chest pain and symptomatic brady-arrhythmia occurred distinctly at different times while she was being closely monitored. Since she had no past history of syncope or history suggestive of brady-arrhythmias and the documented complete heart block and asystole occurred in time sequence of variant angina, it is presumed that the underlying etiology is the same. The electrophysiologic study done during the admission was normal indicating no underlying occult conduction disorder.
This dual mode of presentation is very unusual and to the best of our knowledge not reported earlier. It is likely that different segments of coronary arteries were involved in t spasm at different times. The complete heart block and asystole could have resulted from a spasm of the distal right coronary artery probably AV nodal branch at a time when the proximal vessels did not have a flow limiting spasm.
In untreated patients, during pain and ST elevation, ventricular arrhythmias pose a high risk pf SCD. In one study, 42% of patients experienced serious ventricular arrhythmias during ST elevation.(4) The risk is especially high in mutli-vessel vasospasm. Cardiac arrhythmias, both tachy-arrhythmias (during anterior ST segment elevation) and brady arrhythmias (during inferior ST segment elevation) have been reported during episodes of chest pain (5).
Our patient never manifested with any arrhythmia during ECG changes of ischemia. The multi-vessel spasm was confirmed by angiography though the vessels involved did not show complete occlusion. The treatment with nitrates can explain the absence of complete spasmodic occlusion in the coronary artery segments visualized.
Calcium channel blockers and nitrates are the mainstay of treatment. Aphla-blockers are an alternative. Once started on treatment, the prognosis is good. Beta-blockers are usually avoided. PCI with stent implantation in the spastic segments has been reported in refractory cases (6). Permanent pacemaker implantation for recurrent life threatening brady arrhythmia inspite of nitroglycerine infusion as needed in this patient has not been reported earlier. This therapy besides taking care of the recurrent bradyarrhythmia would also allow liberal use of diltiazem or verapamil which is an important adjunct .
Conclusions
This case illustrates the challenges of diagnosing acute coronary syndromes. Before embarking on fibrinolytic therapy or primary PCI, patients (especially younger females) with episodic chest pain and alarming ST elevation, should be considered for the diagnosis of variant angina and nitroglycerine administration is very important. The case also illustrates that patients may develop life threatening arrhythmias rarely because of vasospasm in absence of chest pain and ischemic ECG changes.
References
1. Prinzmetal M, Kennamer R, Merliss R, et al. Angina pectoris: 1.A variant form of angina pectoris. Am J Med. 1959; 375-88
2. Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomotor reactivity: Differences between Japanese and Caucasian patients. J am coll cardiol 1999; 33: 1442-52
3. Mishra PK. Variations in presentation and various options in management of variant angina. Eur J Cardiothoracic Surg 2006; 29: 748-759
4. Miller DD, Waters DD, Szlachcic J, et al. Clinical characteristics associated with sudden death in patients with variant angina. Circulation. 1982; 66:588-592
5. Chou TC, Knilans TK, eds. Electrocardiography in clinical practice: Adult and. Paediatric. 4th ed. Philadelphia PA, WB Saunders; 1996.
6. Kaul U, Singh B, Fotedar J, Dixit NS. Coronary stenting for refractory coronary vasospasm of proximal left anterior descending artery. J Invas Cardiol 10; 1998 : 95-97
|