Intra Cardiac Mass – A Diagnostic And Therapeutic Dilemma.
Dr Shilpi Mohan,Dr Abhay Kumar,Dr Niraj Kumar,Dr Madhukar Shahi,
Department of Cardiology
Artemis Health Institute , Sector 51, Gurgaon 122001
|
|
INTRODUCTION
Peripartum cardiomyopathy is a rare cause of heart failure with a reported incidence of 1 per 3000 to 1 per 4000 live births and a fatality rate of 20-50% in first year(1). It initially presents with signs and symptoms of congestive heart failure and rarely with thromboembolic complications. We report an unusual case of peripartum cardiomyopathy in a previously healthy postpartum woman who presented with multiple mobile clots in left ventricle which were successfully treated with anticoagulants.
Case report
A 25 years old female presented to our emergency room with complaints of progressively increasing dyspnoea on exertion, paroxysmal nocturnal dyspnoea and orthopnea of 15 days duration. She was not a known case of rheumatic heart disease, congenital heart disease, hypertension, diabetes or cardiomyopathy. She had no febrile illness in the recent past. She had delivered a healthy baby three months back without any complications and was asymptomatic during her last month of pregnancy and early post partum period.
On general examination , she was conscious and had no neurological deficit. Facial puffiness and lower limb pitting edema were noticeable. Her vitals were stable and jugular venous pressure was raised . On cardiovascular examination, LVS3 was present. Bilateral inspiratory crepts were present till mid thoracic region. Transthoracic echocardiography was done which showed global hypokinesia, LVEF 15%. Multiple
 |
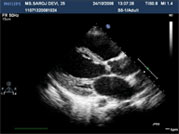 |
| Figure1(a) | Figure2(b) |
 |
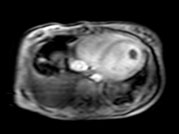 |
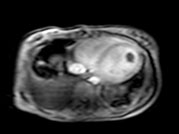
| Figure2(a) | Figure2(b) |
 |
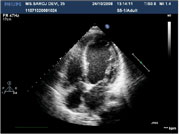 |
| Figure3(a) | Figure3(b) |
Correspondence : Dr (Mrs) Shilpi Mohan Department of Cardiology,
Artemis Health Institute , Sector 51, Gurgaon 122001, Haryana India
Email:shilpi2708@gmail.com, shilpi2708@rediffmail.com
|
Two of the masses showed intramass hypoechogenecity. Mild MR , AR and TR were present and there was evidence of moderate pulmonary arterial hypertension. Cardiac MRI was done to differentiate between clot and tumour so as to plan further management. It suggested multiple intracardiac clots attached to the lateral wall of the left ventricle [Figure 2(a), Figure 2(b)]. Based on the history, clinical examination and non invasive cardiac evaluation, the diagnosis of peripartum cardiomyopathy , severe LV dysfunction with intracardiac clots was made. She was treated with decongestants, anticoagulants. INR was targeted between 2-3 and after stabilization, she was discharged on anti-failure treatment and anticoagulants-LMWH and Acitrom. She was reviewed after 2 weeks. Repeat ECHO showed no improvement in LV systolic function but more than 90% of the clots had resolved [Figure 3(a), Figure 3(b)]. Patient is symptomatically better and has been continued on oral anticoagulants.
DISCUSSION
The differential diagnosis of an intracardiac mass includes thrombus, tumour or vegetation. Some of the anatomical variants mimic such as eustachian valve, chiari network, crista terminalis,
pectinate muscle, right ventricular moderator band or an interatrial septal aneurysm mimic cardiac mass. These normal variants more often involve right sided chambers and are found incidentally. Coronary or an aortic aneurysm, lipomatous hypertrophy of interatrial septum, a hiatus hernia or a catheter / pacemaker lead may also mimic a cardiac mass and are known as “pseudotumours”(2-5). An echo artifact such as the near field clutter, reverberations or a side lobe artifact could also be mistaken for a mass.
Cardiac MRI is a very good imaging tool to differentiate various intracardiac masses. The major advantages of CMR include larger field of view of both cardiac and extracardiac structures, multiplanar 3-D imaging, excellent inherent natural tissue contrast and the ability to characterize tissue with increased water, fat or soft tissue contents by their varying degrees of magnetized T1 or T2 weighted relaxation times. Gadolinium contrast enhancement pattern of increased capillary perfusion help to study the extent of vascularity of a mass(4,5). Thrombus demonstrates increased signal intensity on T1 weighted image due to oxyhemoglobin or deoxyhemoglobin
and lower signal intensity on gradient echo cine images and it does not demonstrate gadolinium contrast enhancement. Chronic thrombi have
uniformly low signal on T2 weighted image compared with a tumour. An organized clot however may demonstrate intermediate heterogenous areas of enhancement that may be mistaken for a cardiac tumour such as a myxoma(6,7). Primary benign cardiac tumour such as lipoma, rhabdomyoma or a fibroma and a hemangioma have variable heterogeneity and signature tissue characteristics that are typical for the individual tumour or CMR imaging(3,4,5). Cardiac MR imaging thus provides a more definitive diagnosis of the cardiac mass and helps to plan appropriate therapeutic strategies for the patients.
Evaluation of the response of the mass to anticoagulation to determine etiologic diagnosis may cause unnecessary delay in diagnosis; whereas surgical resection may be too aggressive an approach or not feasible in several cases.
About one third of the patient with dilated cardiomyopathies have left ventricular thrombi(8).The rate of systemic embolization seen with mobile thrombi is high. Definitive treatment of these intracardiac thrombi are not well established. Oral anti-coagulation has shown a resolution rate of 13-59%(9). Thrombolysis with urokinase, streptokinase and t-PA has been reported but the risk of hemorrhagic or embolic complications are unacceptably high(10).
Surgical thrombectomy can be done but patient with
dilated cardiomyopathies are at increased risk for post operative morbidity and mortality(11). High dose intravenous heparin effectively treats thrombi that are mobile and protrudes into LV cavity. Complete resolution of nearly 83% of thrombi has been documented after a mean of 14 days of treatment.
Very few clinical cases of LV thrombi treated with LMWH have been reported. Recently a preliminary study showed safety and efficiency of Enoxaparin in disappearance or size reduction of LV thrombi associated with acute myocardial infarction or dilated cardiomyopathy. Aspirin and Clopidogrel in combination with LMWH were used in that study but did not show much additional benefit(12). Rahiminejad et al have reported beneficial effect of combination therapy of Enoxaparin and Ticlopidine in treatment of ventricular thrombus in Thalessemia intermedia patients(13). Mallory et al have also reported patient with mobile thrombus who was successfully treated with LMWH(14).
CONCLUSION
In conclusion, MRI is a useful investigative modality to differentiate tumor from LV clots and helps in guiding the management. Anticoagulants
still remain the mainstay in the medical management of such cases with significant clot resolution rate.
REFERENCES
1. Lamport MB, Lang RM: Peripartum cardiomyopathy. AM Heart J.1995, 130:860-70.
2. Reeder GS, Khanderia BK, Seward JB, Tajik AJ. Transesophageal echocardiography and cardiac masses. Mayo clin proc. 1991; 66: 1101-1109.
3. Gulati G, Sharma S, Kothari SS, et al. comparison of echo and MRI in imaging evaluation of intracardiac masses. Cardiovascular intervent radiol.2004;27: 459-469
4. Sparrow PJ, Kurian JB, Jones TR, et al. MR imaging of cardiac tumours. Radiographics .2005;25(5):1255-1276.
5. Hoffmann U, Globits S, Frank H. Cardiac and paracardiac masses. Current opinion on diagnostic evaluation by magnetic resonance imaging. Eur Heart J. 1998;19:553-563.
6. Mollet NR, Dymarkowski S, Volder W, et al. Visualization of ventricular thrombi with contrast enhanced magnetic resonance imaging in patients with ischemic heart disease. Circulation. 2002; 106(23):2873-2876.
Page 11
7. Paydarfar D, Krieger D, Dip N, et al. In vivo magnetic resonance imaging and surgical histopathology of intracardiac masses: distinct features of subacute thrombi. Cardiology.2001; 95(1): 40-47.
8. Gottdiener JS, Gay JA, Van Voorhees L, DiBianco R, Fletcher RD. Frequency and embolic potential of left ventricular thrombus in dilated cardiomyopathy: assessment by 2-dimensional echocardiography. Am J Cardiol 1983; 52: 1281-1285.
9. Heik SCW, Kuper W, Ham C, et al. Efficacy of high dose intravenous heparin for treatment of left ventricular thrombi with high embolic risk. J Am Coll Cardiol 1994; 24:1305-1309.
10. Keren A, Goldberg S, Gottlieb S. Natural history of left ventricular thrombi : their appearance and resolution in the post hospitalization period of acute myocardial infarction. J Am Coll Cardiol 1990; 15: 790-800.
11. Nili M, Deviri E, Jortner R, Strasberg B, Levy M J. Surgical removal of a mobile, pedunculated left ventricular thrombus: report of 4 cases. Ann Thorac Surg 1988; 46: 396-400.
12. Meurin P, Tabet JY, Renaud N, et al. Treatment of left ventricular thrombi with a low molecular weight heparin. Int J Cardiol. 2005;98(2):319-23.
13. Enoxaparin Plus Ticlopidine : An effective combination therapy for intracardiac thrombi in Thalessemia Intermedia . Iran J Pediatr. Mar 2008; Vol 18(No I),Pp 79-82.
14. Treatment of mobile left ventricular thrombus with low molecular weight heparin. NEJM . Volume 341: 1082-1083.
|