Effects of Aspiration Thrombectomy on Mortality in Patients with Acute
Myocardial Infarction Undergoing Primary Percutaneous Coronary
Intervention: A meta-analysis of the randomized trials.
Charan Lanjewar MD,DM, Sanjit Jolly MD, FRCPC, Shamir R. Mehta MD, FRCPC, FACC.
Seth G.S Medical College & KEM Hospital, Mumbai,India (CL)
Mcmaster University and
Poplation Health Research Institute,
Hamilton Health Sciences, Hamilton, Canada
|
|
INTRODUCTION In patients with ST-segment elevation myocardial infarction (STEMI), primary percutaneous coronary intervention (PCI) restores patency of the infarct-related artery in greater than 90% of patients, but myocardial reperfusion at the at the tissue level may often be suboptimal1-3. Reduced myocardial perfusion at the tissue level is is possibly related to distal micro-embolization of thrombus6-9 and worse clinical outcomes.4-5 Therefore, aspiration of thrombus prior to PCI may improve tissue perfusion and clinical outcomes in patients with STEMI. |
METHODS
Search strategy
MEDLINE, CENTRAL and EMBASE were searched for eligible studies between 1990 to February week 4, 2008. In addition, a sensitive search strategy for randomized trials was used from the Cochrane Collaboration. The following key words were used: randomized trial, myocardial infarction, heart infarction, primary angioplasty, thrombectomy, percutaneous coronary intervention. Various combinations of these terms were used based on the database requirements and no language restrictions were placed. Conference abstracts for the American Heart Association, American College of Cardiology, Transcatheter Therapeutics and European Society of Cardiology were hand searched from 2005-2008. Prior systematic reviews were cross referenced to include all studies. Furthermore, oral presentations and/or expert slide presentations were included (searched on TCT [www.tctmd.com], EuroPCR [www.europcr.com], ACC [www.acc.org], AHA [www. aha.org], and ESC [www.escardio.org] Web sites from January 2005 to February 2008).
Email:charanlanjewar@hotmail.com
|
Eligibility Criteria
In order to be included, the study needed to be (1) A randomized trial evaluating aspiration thrombectomy and (2) Included with a patient population of ST segment elevation myocardial infarction treated with primary PCI.
Outcome measures
The primary outcome was mortality at mean follow up. Secondary outcomes included the composite of death, MI or stroke and the composite of death, MI, stroke or target vessel revascularization and bleeding. In addition, we evaluated the proportion of patients in each group with myocardial blush grade 3
(MBG 3), Thrombolysis in Myocardial Infarction (TIMI) flow grade of 3, ST-segment resolution (>50%) after 1 hour of the procedure, distal embolisation, slow flow or no-flow phenomenon. Safety outcomes included rates of coronary perforation, flow limiting dissection and major bleeding.
Data extraction and validity assessment
Data were independently abstracted by 2 investigators. In case of incomplete or unclear data, authors, where possible, were contacted. Disagreements were resolved by consensus.
Statistical Analysis: Data were managed according to the intention- to-treat principle. Odds ratio (OR) and 95% CIs were used as summary statistics. The pooled OR was calculated by using a Mantel-Hanzel fixed effect model . The Breslow-Day test was used to examine the statistical evidence of heterogeneity across the studies ( P <0.1).A sensitivity analysis was performed according to fixed effect model in addition, a linear regression approach to measure funnel plot asymmetry was used. Results are reported as regression coefficients with associated 95% CIs and 2-sided P values. Statistical software “Review Manager (RevMan)[computer Program] Version 5.0 was used 10. The study was performed in compliance with the Quality of Reporting of Meta-analyses guidelines.11
RESULTS
Overall, 1,236 citations were identified of which 18 trials involving 3,879 patients met the inclusion criteria (Figure 1). Of these, 1,948 patients were randomized to aspiration thrombectomy and 1,931 to control. The mean follow up time was 8.9 months. The baseline characteristics of included trials14-31 are shown in Table I. The mean age was 63±13 years in aspiration thrombectomy group and 66±12 years in the control group. All patients had ischemic time less than 24 hours.
 |
Efficacy Outcomes :( Table 2)
Over an average follow up of 8.9 months, there were 53 (2.9%) deaths in the AT group compared with 76 (4.2%) deaths in the control group (OR 0.70, 95% CI 0.49-0.99, P=0.04) (Figure 2). Overall 100 (5.6%) patients in the aspiration thrombectomy group had a death, MI or stroke compared with 126 (7.1%) patients in the control group (OR 0.78, 95% CI 0.60-1.03, P=0.08) (Figure 3). There was a consistent reduction in MI in the AT group (1.86 % vs 2.54%, OR 0.74, 95% CI 0.47-1.16). Stroke rates were low overall at <1%, but non-significantly higher in the AT group (0.78 % vs 0.28 %, OR 2.14, 95% CI 0.92-4.98 ,p=0.08). The composite of death, MI, stroke, bleeding or target vessel revascularization occurred in 196 (11%) patients in the AT group compared with 242 (13.6%) patients in the control group (OR 0.77, 95% CI 0.63-0.99, P=0.01) (Figure 4)
|
Table 2: Summary OR's of Major outcomes at average follow up of 8.9 months.
Death |
18 |
53(2.9%) |
76(4.2%) |
0.70 [0.49- 0.99] |
P=0.04 |
MI |
18 |
33(1.86%) |
45(2.56%) |
0.74 [0.47-1.16] |
P=0.19 |
Stroke |
18 |
14(0.78%) |
5(0.28%) |
2.14 [0.92- 4.98] |
P=0.08 |
Death/MI/Stroke |
16 |
100(5.6%) |
126(7.1%) |
0.78 [0.60- 1.03] |
P=0.08 |
Death/ MI/ stroke /TVR / Bleeding |
18 |
196(11%) |
242(17%) |
0.77 [0.63- 0.95] |
P=0.01 |
Table I: Baseline Characteristics of included trials
Study |
No. of Pt |
Intervention( n) |
Exclusion criteria |
TCL |
Rescue PCI(%) |
GP 2b3a |
Stent |
I-T Min |
Primary outcome |
f/u month |
|
Ali Arshad 2006 15 |
480 |
Angioget(240), |
IT>12 Hr,EF<35%, shock, |
No |
34% |
94.50% |
94% |
200 |
Infarct size |
1 |
|
Andersen 2007 13 |
172 |
Rescue Catheter(87) , Control(85) |
IT>12 Hrs,LBBB, fibrinolytic treatment |
No |
No |
100% |
NR |
NR |
LV Vol,EF |
1 |
|
Antoniucci 2004 20 |
100 |
Angiojet(50), control(50) |
IT>12 Hr; lytic therapy; BBB or PM; IRA <2.5 mm |
No |
No |
98% |
98% |
252 |
STR |
1 |
|
Beran 2002 22 |
61 |
X-sizer (30), control(31) |
IT>12 Hr,Graft; no thrombus visible, open IRA |
Yes |
23% |
73% |
NR |
285 |
TIMI frame count |
1 |
|
B. Chevalier 2007 28 |
249 |
Export Catheter(120), Control(129) |
IT>12Hrs,Lytic therapy , shock , |
No |
No |
65% |
NR |
NR |
MBG ,STR |
12 |
|
Burzotta 2005 18 |
99 |
Diver CE (50), Control(49) |
No Angiographic exclusion criteria, IT>12 Hrs |
No |
32% |
68% |
NR |
NR |
MBG, STR |
1 |
|
De Luca 2006 17 |
68 |
Diver CE(38), Control(38) |
IT > 12Hrs,Previous MI or CABG; |
Yes |
No |
100% |
100% |
408 |
LV Remodelling |
6 |
|
Dudek 2004 24 |
72 |
Rescue(40), Control(32) |
IT>12 Hrs, shock ,IRA <2.5 mm. |
Yes |
No |
0% |
NR |
250 |
MBG 3 flow |
3 |
|
Dudek 2007 27 |
196 |
Diver CE(102), Control(96) |
IT>6 Hrs duration with >1 flow at baseline. |
NR |
No |
62% |
99% |
206 |
STR >70%. |
1 |
|
Kaltoft A 2006 16 |
115 |
Rescue(108), Control(107) |
IT> 12 Hrs,Prior lytic therapy,shock |
No |
No |
96% |
95% |
225 |
Infarct size |
1 |
|
|
355 |
TVAC(180), Control(175) |
IT>24 Hrs,shock,renal faillure,LMCA stenosis |
No |
No |
0% |
93.80% |
294 |
MBG |
24 |
|
Lee 2006 25 |
135 |
Export catheter(67), |
IT>12 Hr., shock,LMCA stenosis |
Yes |
No |
0% |
NR |
NR |
MBG, STR |
1 |
|
Lefevre 2005 19 |
201 |
X-sizer (101), control(100) |
IT>12 Hrs,previous PCI in IRA, rescue PCI, Lvef< 30%, |
Yes |
No |
65% |
NR |
NR |
STR |
6 |
|
Napodano 2003 21 |
92 |
X-sizer(46), control(46) |
IT>12 Hr,LBBB,LMCA lesions, IRA <2.5 mm |
Yes |
No |
43% |
92.40% |
221 |
MBG |
1 |
|
|
50 |
Export Catheter(24), Control(26) |
IT>12 Hr |
No |
29% |
0% |
NR |
312 |
STR |
1 |
|
Sardella G 26b |
175 |
Export Catheter(88), Control(87) |
IT>9 hrs , IRA <2.5 mm , Angiographically No thrombus , T |
Yes |
0% |
100% |
100% |
N409 |
MBG, STR |
9 |
|
|
148 |
Pronto (74), Control(74) |
IT>12 Hr , cardiogenic shock, Prior MI orCABG . |
Yes |
0% |
100% |
99% |
NR |
MBG |
1 |
|
|
1006 |
Export(503), Cotrol(503) |
IT>12 hrs, Rescue PCI |
Yes |
0% |
93% |
92% |
190 |
MBG |
12 |
( where , IT-Ischemic Time, F/U-Follow Up, TCL-Thrombus Containing Lesion, GP 2b3a-GP IIB-IIIA Inhibitors, MBG-Myocardial Blush Grade, STR-ST segment resolution)
|
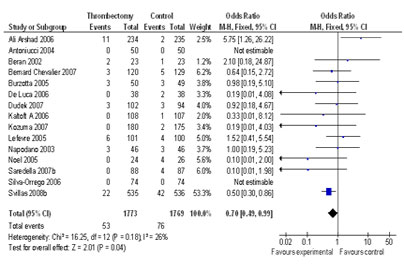 |
Figure 2.Forest plot of comparison of Mortality (Primary Outcome) in Aspiration Thrombectomy vs.control at long term available follow up of 8.9 months. |
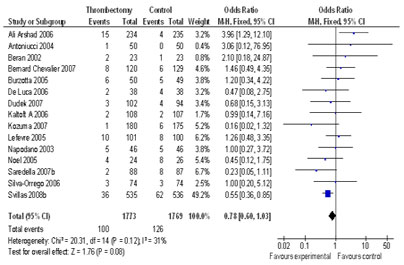 |
Figure3: Forest plot of comparison of combined outcome of Mortality, MI and Stroke in Aspiration Thrombectomy vs.control at long term available Follow up of 8.9 months. |
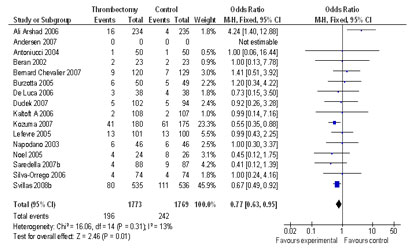 |
Figure 4.Forest plot of comparison of Composite of death, MI, stroke, target vessel revascularization and bleeding in Aspiration Thrombectomy vs.control at long term available follow up of 8.9 months. |
Outcom |
Studies |
Aspiration Thrombectomy |
Control.
|
OR |
95% CI |
P value |
Major Bleeding |
18 |
38/1773(2.40%) |
44/1769(2.48%) |
0.86 |
[0.56-1.34] |
P=0.51 |
Coronary Perforation & or Flow Limiting Dissections |
13 |
11/1678(0.6%) |
10/1672(0.5%) |
1.08 |
[0.48- 2.43] |
P=0.84 |
Safety Outcome
Data on coronary perforations & or flow limiting dissections were available in 3,350 (86.3%) of patients. There was no difference in the rates of perforation & or flow limiting dissections between the groups (0.6% AT vs 0.5% control, OR 1.08 CI 0.48- 2.43, P = 0.84). Major bleeding was similar between the groups (2.4% vs 2.48%, OR 0.86, 95% CI 0.56-1.34,P=0.51) (Table 3)
Other Outcomes (Table 4)
AT was associated with a significantly higher rate of postprocedural MBG 3 ( 50.39% vs 34.26%, OR 2.01; CI 1.74 - 2.31,P < 0.00001) and TIMI 3 flow (85.82% vs 81.54% , OR 1.42; CI 1.17 -1.72 ,P = 0.0004) compared with control. AT was also associated with a significant reduction in distal embolization ((6.08% vs 11.22%, OR 0.51; 0.37 - 0.70, P< 0.0001).
AT was associated with a significant reduction in ST Resolution (> 50%) after the procedure compared with control therapy (60.20% vs 40.24% , OR 2.40,CI 2.08- 2.78, P < 0.00001).
Total procedural time data was available in 1696 patients (43.8%). It was slightly longer with AT (mean difference of 5.88 minutes, 95% CI 3.71- 8.05].
DISCUSSION:
The main finding of our study is that the addition of aspiration thrombectomy to primary percutaneous coronary intervention in patients with acute ST segment elevation myocardial infarction reduces mortality by about one-third compared with primary percutaneous coronary intervention alone. This benefit in mortality was associated with a higher proportion of patients receiving aspiration thrombectomy with complete ST segment resolution, improved TIMI 3 flow involving the infarct related vessel and improved tissue perfusion as assessed by myocardial blush grade. The rates of re-MI and stroke were not significantly different between the groups. From a safety perspective, there was no increase in the rate of coronary artery perforation or major bleeding and only a modest increase in prodecural time with aspiration thrombectomy. Thus, our data suggest that aspiration thrombectomy is a useful procedure that should be considered in all patients with STEMI undergoing primary PCI.
The benefit of aspiration thrombectomy was predicated on the assumption that by aspirating the thrombus in the disrupted plaque distal embolization of thrombus would be prevented, resulting in improved tissue perfusion. Our meta-analysis demonstrated less distal embolization of thrombus and improved measures of early infarct related artery patency including more rapid ST segment resolution and a higher proportion of patients with TIMI grade 3 flow. These benefits lead to improve myocardial tissue perfusion as demonstrated by a greater proportion of patients with myocardial blush grade 3 with aspiration thrombectomy. All of these benefits likely translated into the reduction in mortality observed in this study.
|
Table 4: Summary OR's of surrogate outcomes at average follow up of 8.9 months.
Outcome |
Studies |
Aspiration |
Control |
Statistical Methods |
Effect Estimates |
P value |
Post procedural MBG 3 flow |
15 |
866/1722 |
586/1710 |
Odds Ratio |
2.01 |
P <0.00001 |
Postprocedural TIMI flow |
15 |
1483/1728 |
1396/1712 |
Odds Ratio |
1.42 |
P<0.0004 |
> 50% ST resolution 1 hour after procedure |
16 |
994/1651 |
679/1687 |
Odds Ratio |
2.40 |
P<0.00001 |
Distal embolization of thrombus |
10 |
64/1052 |
117/1141 |
Odds Ratio |
0.51 |
P<0.0001 |
No flow/Slow flow |
13 |
40/1153 |
77/1115 |
Odds Ratio |
0.51 |
P<0.0006 |
Infarct size by peak CK-MB value(ugm/ltr) |
6 |
NA |
NA |
Mean Difference |
-12.67 |
P=0.08 |
Total procedural time in minutes |
12 |
NA |
NA |
Mean Difference |
5.88 |
P=0.93 |
Table 4: Comparison of the findings of this study with selected studies from India*
First author |
Year |
Place |
Urban |
Age |
Sample |
Overall prevalence |
Diagnosis by history (men) |
Diagnosis by ECG (men) |
Definite |
Mathur 16 |
1960 |
Agra |
Urban |
NA |
1046 |
1.05 |
|
|
|
Padmavati 17 |
1962 |
Delhi |
Urban |
NA |
1642 |
1.04 |
|
|
|
Chaddha 14 |
1990 |
Delhi |
Urban |
25-64 |
13723 |
9.67 |
3.95 |
5.63 |
|
Kutty 10 |
1993 |
Kerala |
Rural |
>25 |
1130 |
7.43 |
|
|
1.4 |
Gupta 15 |
1995 |
Jaipur |
Urban |
>20 |
2212 |
6 |
|
3.5 |
|
This study |
2004-5 |
Dharan, |
Urban |
≥35 |
1000 |
5.7 |
3.6 |
2.4 |
2.1 |
* Adapted from Gupta et al. South Asian J preventive cardiology 1997; 1: 27-32. NA: information not available
Our study demonstrates that aspiration thrombectomy is safe, with no increase in coronary perforation or flow limiting dissections in major bleeding. However, there was an increase in procedural time (mean 5.8 minutes), but this modest increase did not seem to have a detrimental effect. The rate of stroke overall was low, but non-significantly higher in the aspiration thrombectomy group. Whether this result is real or the play of chance cannot be addressed with the current data.
Our results demonstrating a reduction in mortality with aspiration thrombectomy are in contrast to trials evaluating distal protection devices, where no reduction in infarct size or improvement in event-free survival has been observed 31 . Randomized studies and guidelines do not support routine use of distal embolic protection with primary PCI in all STEMI patients for reduction of major adverse cardiac event rates. 32
Additional factors must be considered in the interpretation of the results of the current meta-analysis. Strict inclusion criteria in most of the trials led to the exclusion of high-risk patients, such as those with advanced Killip class and cardiogenic shock at presentation. In fact, these patients might have been benefited most from mechanical devices in terms of enhanced perfusion and better survival, given the higher rates of distal embolization and poor perfusion observed in these conditions.33 Similarly other meta-analysis also demonstrated improved reperfusion and mortality in AMI.34-37
Furthermore, angiographic evidence of thrombus was not required in most of trials, and it is possible that adjunctive mechanical devices are still effective irrespective of the thrombus burden.
The concordance between enhanced myocardial perfusion (better MBG 3 flow,>50% ST resolution) and improved survival at long term follow up is perhaps not unexpected. We expected smaller infarct size in treatment group but indeed we found that it was not statistically different between two groups. This could be because this data was only available in few trials. Increased infarct size was seen in two studies. It must be kept in mind that estimation of infarct size was done by CK-MB value and data was only available in 16% cases. We have not analysed the infarct size estimation by SPECT and MRI as it was only done in few trials. It is certainly possible that the increased infarct size seen in the study by Kaltoft and colleagues with aspiration thrombectomy and the increased infarct size seen in AiMI with rheolytic thrombectomy could be related to distal embolization at the time of thrombectomy.15, 16
This meta-analysis was not performed on individual patient data as complete data sets were not available. Data on slow flow-No-flow, distal embolization, infarct size, long term mortality and MACE were not available in some trials. However, it is unlikely that an individual patient data meta-analysis would result in a different outcome.
CONCLUSION: In patients undergoing primary PCI, the addition of aspiration thrombectomy reduces both mortality and recurrent ischemic events at follow up of 8.9 months .These benefits are associated with improved measures of infarct-related artery patency, better myocardial perfusion, and less distal embolization.
|
RERERENCES:
1. Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction:a quantitative review of 23 randomised trials. Lancet 2003; 361:13- 20.
2. Zhu MM, Feit A, Chadow H, et al. Primary stent implantation compared with primary balloon angioplasty for acute myocardial infarction: a meta-analysis of randomized clinical trials. Am J
Cardiol 2001; 88:297 - 301.
3. De Luca G, Suryapranata H, Stone GW, et al. Abciximab as adjunctive therapy to reperfusion in acute ST-segment elevation myocardial infarction: a meta-analysis of randomized trials. JAMA 2005; 293:1759 - 65.
4. Van’t Hof AW, Liem A, Suryapranata H, et al. Angiographic assessment of myocardial reperfusion in patients treated with primary angioplasty for acute myocardial infarction. Circulation 1998; 97:2302 -6.
5. De Luca G, van’t Hof AW, Ottervanger JP, et al. Unsuccessful reperfusion in patients with ST-segment elevation myocardial infarction treated by primary angioplasty. Am Heart J 2005; 150:557 - 62.
6. Henriques JP, Zijlstra F, Ottervanger JP, et al. Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur Heart J 2002; 23:1112 -7.
7. Ischinger T, X-SIZER Study Group. Thrombectomy with the X-SIZER catheter system in the coronary circulation: initial results from a multi-center study. J Invasive Cardiol 2001; 13:81 -8.
8. Hamburger JN, Serruys PW. Treatment of thrombus containing lesions in diseased native coronary arteries and saphenous vein bypass grafts using the AngioJet Rapid Thrombectomy System. Heart 1997;22:318 - 21.
9. Carlino M, De Gregorio J, Di Mario C, et al. Prevention of distal embolization during saphenous vein graft lesion angioplasty.Experience with a new temporary occlusion and aspiration system.Circulation 1999; 99:3221 -3.
10.Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.0 [updated February 2008]. The Cochrane Collaboration, 2008. Available from www.cochrane-handbook.org.
11. Moher D, Cook DJ, Eastwood S, et al. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet 1999; 354:1896- 900.
12.Svilaas T. Vlaar PJ. van der Horst IC. Diercks GF. de Smet BJ. van den Heuvel AF. Anthonio RL. Jessurun GA. Tan ES. Suurmeijer AJ. Zijlstra F. Thrombus aspiration during primary percutaneous coronary intervention. New England Journal of Medicine 2008;358(6):557-67,.
13. Andersen NH. Karlsen FM. Gerdes JC. Kaltoft A. Sloth E. Thuesen L. Botker HE. Poulsen SH. No beneficial effects of coronary thrombectomy on left ventricular systolic and diastolic function in patients with acute S-T elevation myocardial infarction: a randomized clinical trial. Journal of the American Society of Echocardiography 2007; 20(6):724-30.
14. Silva-Orrego P. Colombo P. Bigi R. Gregori D. Delgado A. Salvade P. Oreglia J. Orrico P. de Biase A. Piccalo G. Bossi I. Klugmann S. Thrombus aspiration before primary angioplasty improves myocardial reperfusion in acute myocardial infarction: the DEAR-MI (Dethrombosis to Enhance Acute Reperfusion in Myocardial Infarction. Journal of the American College of Cardiology 2006; 48(8):1552-9.
15. Ali, Arshad. Cox, David. Dib, Nabil. Brodie, Bruce. Berman, Daniel. Gupta, Navin. Browne, Kevin. Iwaoka, Robert. Azrin, Michael. Stapleton, Dwight. Setum, Cindy. Popma, Jeffrey. AIMI Investigators. Rheolytic thrombectomy with percutaneous coronary intervention for infarct size reduction in acute myocardial infarction: 30-day results from a multicenter randomized study. Journal of the American College of Cardiology 2006; 48(2):244-52.
16. Kaltoft A. Bottcher M. Nielsen SS. Hansen HH. Terkelsen C. Maeng M. Kristensen J. Thuesen L. Krusell LR. Kristensen SD. Andersen HR. Lassen JF. Rasmussen K. Rehling M. Nielsen TT. Botker HE. Routine thrombectomy in percutaneous coronary intervention for acute ST-segment-elevation myocardial infarction: a randomized, controlled trial. Circulation 2006;114(1):40-7.
17. De Luca L. Sardella G. Davidson CJ. De Persio G. Beraldi M. Tommasone T. Mancone M. Nguyen BL. Agati L. Gheorghiade M. Fedele F. Impact of intracoronary aspiration thrombectomy during primary angioplasty on left ventricular remodelling in patients with anterior ST elevation myocardial infarction. Heart 2006;92(7):951-7.
18. Burzotta F. Trani C. Romagnoli E. Mazzari MA. Rebuzzi AG. De Vita M. Garramone B. Giannico F. Niccoli G. Biondi-Zoccai GG. Schiavoni G. Mongiardo R. Crea F. Manual thrombus-aspiration improves myocardial reperfusion: the randomized evaluation of the effect of mechanical reduction of distal embolization by thrombus-aspiration in primary and rescue angioplasty (REMEDIA) trial. Journal of the American College of Cardiology 2005; 46(2):371-6.
19. Lefevre T. Garcia E. Reimers B. Lang I. di Mario C. Colombo A. Neumann FJ. Chavarri MV. Brunel P. Grube E. Thomas M. Glatt B. Ludwig J. X AMINE ST Investigators. X-sizer for thrombectomy in acute myocardial infarction improves ST-segment resolution: results of the X-sizer in AMI for negligible embolization and optimal ST resolution (X AMINE ST) trial. Journal of the American College of Cardiology 2005; 46(2):246-52.
20. Antoniucci, David. Valenti, Renato. Migliorini, Angela. Parodi, Guido. Memisha, Gentian. Santoro, Giovanni Maria. Sciagra, Roberto. Comparison of rheolytic thrombectomy before direct infarct artery stenting versus direct stenting alone in patients undergoing percutaneous coronary intervention for acute myocardial infarction. American Journal of Cardiology 2004; 93(8):1033-5.
21. Napodano M. Pasquetto G. Sacca S. Cernetti C. Scarabeo V. Pascotto P. Reimers B. Intracoronary thrombectomy improves myocardial reperfusion in patients undergoing direct angioplasty for acute myocardial infarction. Journal of the American College of Cardiology 2003;42(8):1395-402.
22. Beran G. Lang I. Schreiber W. Denk S. Stefenelli T. Syeda B. Maurer G. Glogar D. Siostrzonek P. Intracoronary thrombectomy with the X-sizer catheter system improves epicardial flow and accelerates ST-segment resolution in patients with acute coronary syndrome: a prospective, randomized, controlled study. Circulation 2002; 105(20):2355-60.
23. Ken Kozuma,Yuji Ikari,Masami Sakurada,Shigeo Kawano,Takaaki Katsuki ,et.al. Long-term Clinical Follow-up in ST Elevation Acute Myocardial Infarction (STEMI) Patients With Thrombus Aspiration Prior to coronary Intervention, 2-year Results of The Vampire Study. Circulation. 2007;116(suppl II):378.
24. Dariusz Dudek, Waldemar Mielecki, Jacek Legutko, Michał Chyrchel, Danuta Sorysz, Satnisław Bartuś, Łukasz Rzeszutko, Jacek Dubiel.Percutaneous thrombectomy with the RESCUE system in The myocardial Infarction. Kardiol Pol 2004; 61: 523-528.
25. Sung Yun Lee; Joon Hyung Doh; June Namgung; et al. TSUNAMI study investigators Export Aspiration Catheter Thrombosuction Before Actual Primary PCI in AMI: TSUNAMI . Circulation 2006;114,18 (Supplement:II):597 .
26 .Gennaro Sardella; Massimo Mancone; Raffaele Scardala; Leonardo De Luca et al.
Impact of Thromboaspiration during Primary PCI on Microvascular Damage and Infarct Size: Acute and Long term ce-MRI Evaluation.Circulation. 2007;116:(suppl II):674.
26 b. Gennaro Sardella.Impact of Thrombectomy with EXPort catheter in Infarct Related
Artery on procedural and clinical outcome in patients with AMI ( EXPIRA Trial ). http://www.crtonline.org/flash.aspx?PAGE_ID=4761
27. Dudek D.Polish-Italian-Hungarian Randomized ThrombEctomy Trial. Presented at TCT 2007 conference (PIHRATE trial).http://www.tctmd.com/show..aspx?id=656
.http://www.crtonline.org/flash.aspx?PAGE_ID=4760
28. Bernard Chevalier .EXPORT Study First report :Presented at TCT 2007 conference. http://www.tctmd.com/show.aspx?id=656
http://www.google.com/search?q=cache:qKvSmr1UAWQJ:clintrialresults.org/Slides/EXPORT.ppt+TCT+2007+-EXPIRA+STUDY&hl=en&ct=clnk&cd=7&gl=ca
29.Noel B,Morice MC,Levefre T,et al.. Thromboaspiration in acute ST elevation MI improoves myocardil reperfusion.. Circulation 2005;112(supplIII):519.
30. Felix Zijlstra, Svillas T . TAPAS: Thrombus Aspiration Shows Impressive Results During PCI for STEMI. One-year data were presented at the Society for Cardiovascular Angiography and Interventions -American College of Cardiology (SCAI-ACC) 2008 joint meeting at Chicago .
http://www.tctmd.com/show.aspx?id=66956
31. George W. Vetrovec, M.D.Improving Reperfusion in Patients with Myocardial Infarction .N Engl J Med 2008; 358;634-637.
32. Giuseppe De Luca, MD,a,f Harry Suryapranata, MD,b Gregg W. Stone, MD,c David Antoniucci et al. Adjunctive mechanical devices to prevent distal embolization in patients undergoing mechanical revascularization for acute myocardial infarction:A meta-analysis of randomized trials. Am Heart J 2007;153:343253.
33. De Luca G, van’t Hof AW, de Boer MJ, et al. Impaired myocardial perfusion is a major explanation of the poor outcome observed in patients undergoing primary angioplasty for ST-segment–elevation myocardial infarction and signs of heart failure. Circulation 2004;109:958 - 61.
34. De Luca G, Dudek D, Sardella G, et al.Adjunctive manual thrombectomy improves myocardial perfusion and mortality in patients undergoing primary percutaneous coronary intervention for ST-elevation myocardial infarction: a meta-analysis of randomized trials [epub ahead of print] [Record Supplied By Publisher].Eur Heart J (England) 5 sept 2008: p S1522-9645.
35.Bavry AA, Kumbhani DJ, Bhatt DL.Role of adjunctive thrombectomy and embolic protection devices in acute myocardial infarction: a comprehensive meta-analysis of randomized trials .[epub ahead of print] [Record Supplied By Publisher]Eur Heart J (England), Sep 23 2008, p S1522-9645.
36. Burzotta F, Testa L, Giannico F, et al.Adjunctive devices in primary or rescue PCI: a meta-analysis of randomized trials. Int J Cardiol 2008; 123(3):313-21.
37. Kunadian B, Dunning J, Vijayalakshmi K, et al.Meta-analysis of randomized trials comparing anti-embolic devices with standard PCI for improving myocardial reperfusion in patients with acute myocardial infarction. Catheter Cardiovasc Interv 2007; 69(4) :488-96.
|